By Colin Konschak, FACHE and Dave Levin, MD
A Framework for Innovation
As noted in part one of our series, we believe the opioid crisis is an “All Hands-On Deck” moment and health IT (HIT) has a lot to offer. Given the many different possibilities, having a method for organizing and prioritizing potential IT innovations is an important starting point. We have proposed a framework that groups opportunities based on an abstract view of five types of functionality. In this article, we will explore the role of technologies that provide clinical decision support.
Clinical Decision Support for Opioid Management
The digitalization of health care via deployment of electronic health records (EHRs) set the stage for clinical decision  support (CDS). In the broadest terms, the goal of CDS is to “make it easy to do the right thing, hard to do the wrong thing.” Classic examples include automated checks for interactions or allergies when a new medication is prescribed. In addition to this kind of alerting, CDS can leverage other IT tools including order sets, care paths, documentation templates, and increasingly, analytics including the advanced analytics of prediction, simulation and pattern recognition.
support (CDS). In the broadest terms, the goal of CDS is to “make it easy to do the right thing, hard to do the wrong thing.” Classic examples include automated checks for interactions or allergies when a new medication is prescribed. In addition to this kind of alerting, CDS can leverage other IT tools including order sets, care paths, documentation templates, and increasingly, analytics including the advanced analytics of prediction, simulation and pattern recognition.
These basic tools can be used in a variety of ways to address the opioid epidemic. Order sets and care paths can be designed and deployed to standardize management and reduce risk in common opioid-use scenarios. Order level checks can guide dosing and check for harmful interactions. Documentation templates can be used as both a prompt to remind clinicians to document key opioid-abuse related information and to streamline the documentation process itself. These types of technology are particularly well suited for well-defined, discrete episodes of care for commonly-occurring conditions like joint replacement or back surgery. Their utility can be limited in complex cases and situations where diagnosis and treatment are highly variable. Fortunately, the emergence of advanced analytics holds lots of promise for addressing more personalized situations.
Advanced Analytics
We are at the dawn of big data in healthcare as clinical data sets develop the volume, velocity and variety required for advanced analytics. Pattern recognition, simulation and predictive analytics hold great promise for medicine in general and should be leveraged to address the crisis. For example, it is increasingly common to see algorithms that predict future risk, outcomes and the potential impact of different therapeutic interventions. It should be possible to apply this to individual patients to predict the best course of treatment for pain, minimize the risk of developing addiction or abusing medications, and recommend the best interventions when patients get into trouble.
The Future is Now: Risk Prediction and Decision Support
Advanced analytics embedded in applications like Venebio Opioid AdvisorTM (VOATM) make them powerful new tools in the fight against opioid abuse. VOA is a validated risk index and clinical decision support tool that can predict future risk of prescription opioid overdose and provide evidence-based guidance to support safer prescribing and risk reduction. A proprietary algorithm produces a personalized risk score that predicts the likelihood the patient will overdose on prescription opioids. The patient’s risk score and predicted probability of overdose is based on multiple patient-specific demographic and clinical variables which are compared with data from tens of millions of opioid-treated individuals.
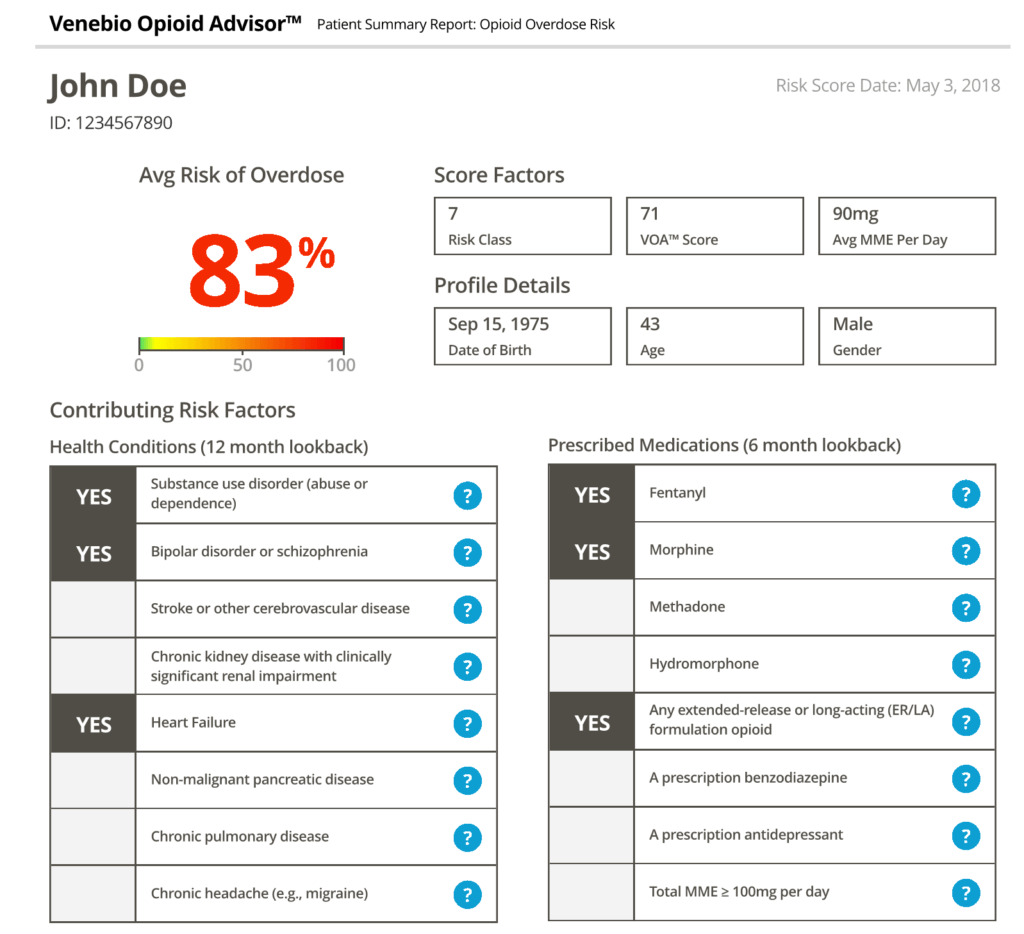
In a recent peer-reviewed publication, VOA showed 90% accuracy in predicting overdose events in a study population of 18.3 million patients who were prescribed opioids.1 Clinicians can also trend data for individual patients over time and get population-level reports that summarize opioid use for groups of patients.
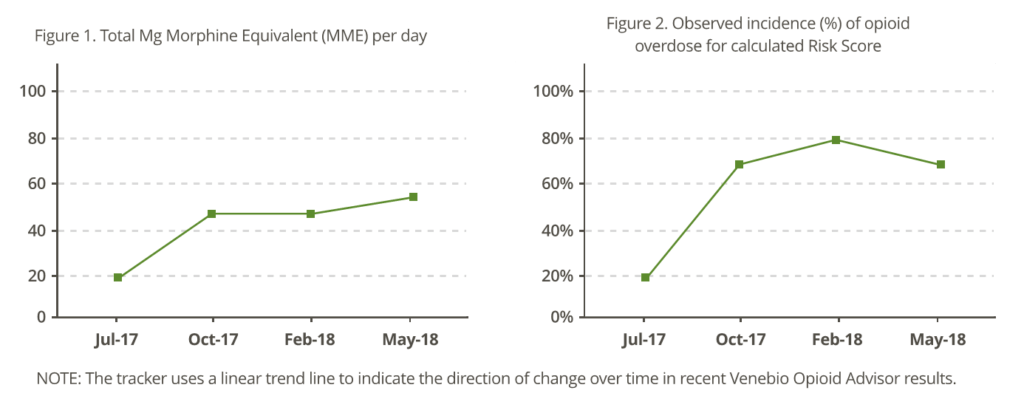
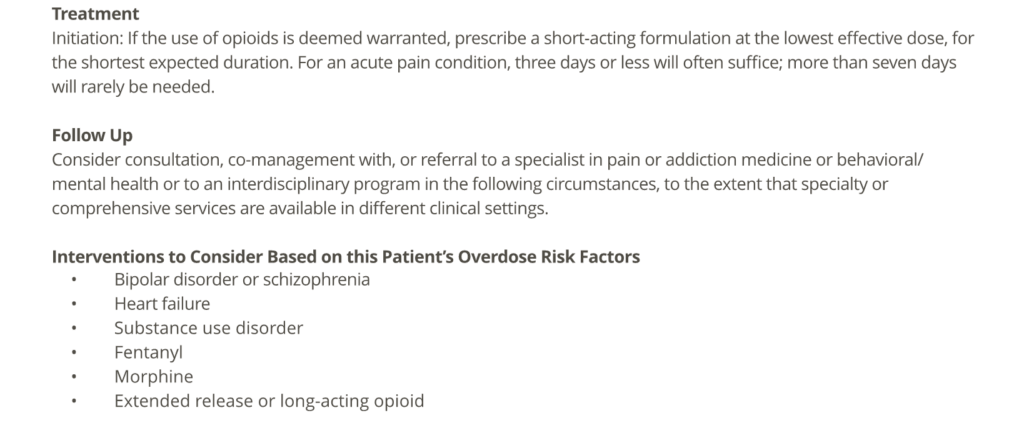
VOA also provides clinical decision support in the form of personalized, evidence-based guidance for reducing the patient’s overdose risk. Clinicians are given specific risk-mitigating interventions to consider when formulating the patient’s treatment plan. A patient-friendly version is also available, which may be used for patient counseling, informed consent, and patient education.
Coming soon to an Electronic Health Record (EHR) Near You?
As noted in previous articles, for CDS technologies to be effective, they must be easy to use. Awkward and time-consuming workflows can be an enormous barrier to adoption and regular use. In most cases, this means tight integration with the EHRs that clinicians commonly use when caring for patients.
This is not a trivial undertaking. It requires careful planning and design that leads to effective integration into the clinical, EHR-based, workflow. It must be easy to access CDS tools; data should flow seamlessly back and forth, with little or no intervention by the end-user, and duplicate data entry must be studiously avoided. Reports, graphs and the like should be visually appealing and intuitive. In summary, decision support has to be woven into the system and presented in ways that support end-user adoption by enhancing clinician access to information and advice and making it easy to incorporate this into their plan of care and documentation.
What’s Next
The next article in this series will look at the role technology can play in managing allocation of scarce resources and expanding access to services like medication assisted therapy (MAT).
References
1 Barbara K Zedler, William B Saunders, Andrew R Joyce, Catherine C Vick, E Lenn Murrelle; Validation of a Screening Risk Index for Serious Prescription Opioid-Induced Respiratory Depression or Overdose in a US Commercial Health Plan Claims Database, Pain Medicine, Volume 19, Issue 1, 1 January 2018, Pages 68–78, https://doi.org/10.1093/pm/pnx009
About the Authors
Dr. Dave Levin has been a physician executive and entrepreneur for more than 30 years. He is a former Chief Medical Information Officer for the Cleveland Clinic and serves in a variety of leadership and advisory roles for health care IT companies, health systems and investors. You can follow him @DaveLevinMD or email DaveLevinMD@gmail.com.
Colin Konschak, RPh, MBA, FACHE is the Chief Executive Officer at Divurgent. Colin is a Registered Pharmacist and is a highly accomplished executive with over 20 years of experience with extensive experience in health care operations, P&L management, account management, strategic planning and alliance management. You can follow him on LinkedIn or email him at ck@divurgent.com.


