by Brent Girardeau
Ruling
In November 2019, the Centers for Medicare and Medicaid Services (CMS), an agency within the Department of Health and Human Services (HHS), issued a final rule defining “standard charges,” delineating hospitals’ publication requirements and laying out an enforcement scheme. (Linked here)
What is Price Transparency?
For years, the federal government has been pushing hospitals to provide greater Medicare price transparency. Provider organizations and supporting lobbyists have maintained that this places an undue burden and competitive disadvantage to hospitals. On Tuesday, June 23rd,2020, the federal court ruled in favor of the Department of Health and Human Services to enforce guidelines of the Affordable Care Act requiring provider organizations to publish the “standard charges for items and services provided by the hospital”.
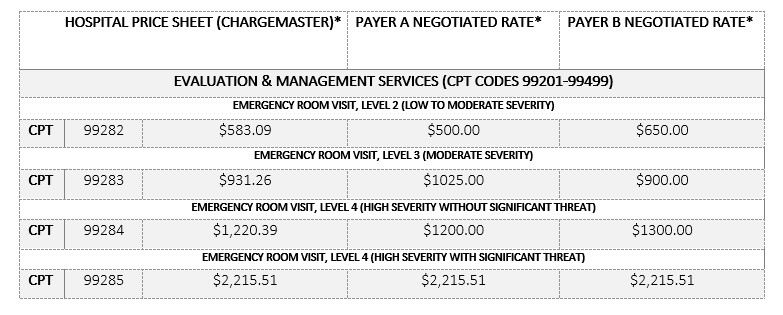
In layman’s terms, hospitals must expand what is made available to the public beyond the charges on a patient bill, but now additionally publish the prices negotiated across all payers and plans for services and items. While some tactical aspects of this are challenging, the bottom line is that it is hard to perceive the strategic value hospitals will gain by publishing the variation in prices charged for service across payers.
Sample “Price Sheet”
*Prices vary by hospital and region. Values not intended to represent actual costs.
**Patient responsibility is determined by the insurance plan.
***Self Pay rates may not reflect chargemaster rates.
Hospital Position on Price Transparency
Hospital representation has contended the language “standard charges” was intended to mean only the chargemaster which generally represents what the patient is charged or would expect to see on a bill. Additionally, many states have passed legislation requiring chargemaster visibility already. However, this does not give visibility to the different rates negotiated for items and services across various payers and plans. One would assume this presents a competitive disadvantage to hospital negotiations with payers on rates. However, it could also have a leveling effect on the competitive landscape with competing hospital systems.
Opportunity or Burden?
The AHA will continue to challenge this ruling, although, under normal circumstances, the appeal would not be heard until after the effective date to be compliant. Assuming this change is impending, and the ruling will stand, the question may be whether to approach compliance as a burden and do the minimum or to utilize it as an opportunity to be early to market with meaningful data that is engaging to the consumer base. The data at the center of the debate is confusing, easily obfuscated, and certainly hard for the average consumer to understand, which may create a customer acquisition opportunity for this to invest early and release a viable product, commercially or internally.