by Steve Weichhand
Healthcare eagerly adopted the continuous improvement programs that transformed the manufacturing industry. Unfortunately, these programs haven’t yielded the same results in healthcare as in manufacturing. Why? Unlike in manufacturing, healthcare lacks efficient tools to monitor and control a critical factor in process improvement: variation. Today, the availability of EHR usage data presents a significant opportunity for healthcare to change this dynamic by targeting and reducing unnecessary variation.
Process Flow and Variation Overview
To understand the importance of variability, we first must establish a high-level understanding of process flows. Just like in manufacturing, healthcare takes a series of inputs and generates an output. Cycle time is the amount of time it takes an individual job to move through queues and processes.
Figure 1: Basic Process Diagram
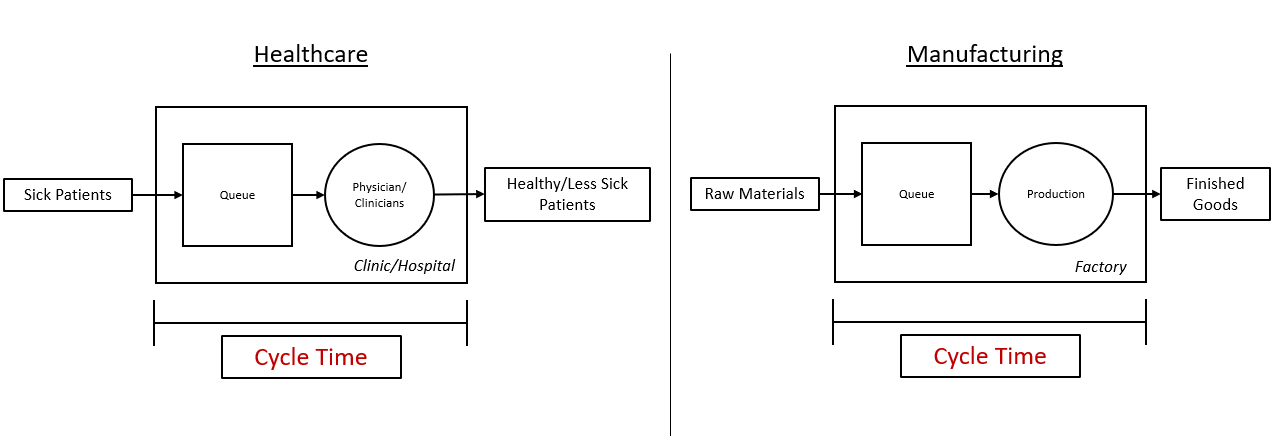
Variability in cycle time arises due to unpredictable yields, glitches in human behavior, unreliable equipment, and many other factors. For resource-constrained systems, like healthcare, queuing times can be very long compared to processing times when variability is introduced. Long cycle times manifest themselves in a variety of ways in healthcare, including long wait times and physician EHR charting after hours.
Unfortunately, it’s difficult to identify and reduce variation and accept that not all variation can be eliminated. Dr. W Edwards Deming, whose ideas shaped the Toyota Production System (TPS) commonly known as Lean, identified two types of variation: common cause and special cause.
- Common Cause. The result of natural patterns that are usual, historical, and quantifiable within a system; there is not much you can do about this type. Examples of common cause include:
- Patient acuity, diagnosis. and comorbidities
- Seasonal or daily demand changes
- No shows or late arrival to appointments
- Special Cause. Due to a defect, unusual, or unpredictable cause. This type of variation can be reduced or eliminated. In healthcare, special cause variation is often a result of individual physicians or clinicians not following best practices. Examples of special cause include:
- Inventory shortage
- Not leveraging EHR shortcuts
- Medication administration error
Monitor EHR-Use Variation
Traditional methods for standardizing physician workflows include training “best practice” workflows through meetings, tip sheets, and/or web-based trainings. Except for certain patient safety or important organizational initiatives, health systems generally do not report on or follow up on adherence to specific best practice recommendations. Not surprisingly, this approach is ineffective at ensuring a low variability in individual physician workflows.
As an alternative to traditional methods, EHR usage data is now available to monitor actual physician behaviors. If harnessed appropriately, this information can enhance a health system’s ability to identify and react to special cause variation for individual physicians. At first thought, this may sound eerily like Big Brother from George Orwell’s book 1984, but this information can benefit patients, physicians, and health systems. For example, organizations can now track:
- Afterhours charting (charting from 7 PM – 7 AM)
- Shortcuts used (ex. personalized orders)
- Average time spent documenting notes per patient
- Average time spent placing orders per patient
- In basket message volume and response time
- Average length of notes
- Average number of orders placed
In a silo, each piece of information listed above is not very helpful but aggregating the data and drawing comparisons to peers within the same specialty highlights valuable improvement opportunities. Any physician outside control limits, or a reasonable deviation from the mean, should be identified and approached with a tailored plan for improvement. In our experience, the physicians who fall outside these control limits are typically unaware of key features or haven’t personalized the EHR.
Reducing Variation
A tailored training program for a significant number of physicians sounds daunting, but it shouldn’t be. Leveraging the EHR-usage data described above allows you to work smarter, not harder. Your physician efficiency program can be scaled up or down based on resources available. You could, for example, focus on the lowest 5% performing internal medicine physicians within the notes activity. Once complete, you could move to the next 5% and so on.
Figure 2: Example Distribution of EHR Time Documenting Notes
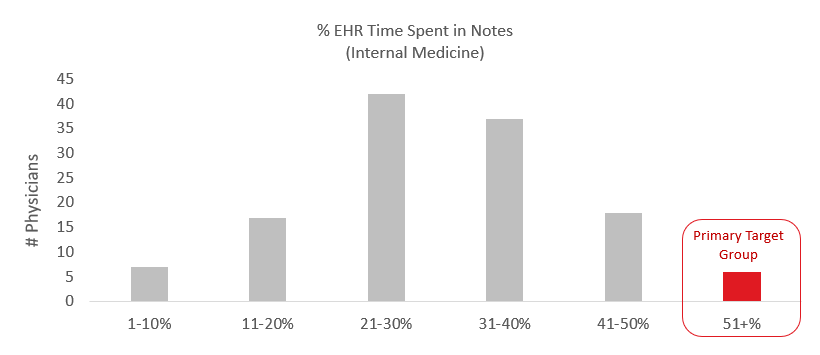
The most direct and immediate way to improve physician’s efficiency in the EHR is to pair them with a physician who is an expert in the system. Once paired, the peer-to-peer physician trainers should assist with system personalization in notes, order entry, clinical review, voice recognition, and other activities in the EHR.
To further reduce variance between physicians, the most successful organizations also leverage usage data to prioritize EHR enhancements. Order sets, note templates, and voice recognition tools have long been thought of as a way to reduce variance between physician workflows, but at many organizations, poor monitoring and maintenance of these tools have resulted in low or nonexistent utilization. Now, with usage data more readily available, links can be made to highly efficient physicians and what order sets or note templates they use or have personally customized. This information can be used to revive order sets or share tools that struggling physicians didn’t know existed.
Summary
If health systems focus on reducing controllable variation, they would be empowered to deliver higher quality, more cost-effective care while also reducing physician burnout. Specifically, considering physicians spend nearly half of their day in the EHR and have made it loud and clear they dislike the inefficient administrative burden of EHR documentation, EHR usage data presents a significant opportunity to reduce unnecessary variation.
Leveraging EHR-usage data and a combination of tailored peer-to-peer training and EHR enhancements is a low hanging fruit opportunity for healthcare to bend the cost curve, improve outcomes, and increase physician satisfaction. Understanding how to harness EHR-usage data to, and the importance of, reducing variation should be a priority of performance improvement teams across the country.


